Interoperability can be dubbed as a data superhighway, but the majority of healthcare stakeholders are still stuck in a parking lot. Integrating and utilizing EHRs together are the first baby steps. Healthcare Interoperability will be an ongoing challenge for healthcare stakeholders due to the industry’s unique information exchange requirements and stringent compliance mandates. If we aim to overcome these hurdles, then achieving 100% EHR interoperability is the final summit where we are yet to reach.
Data Belongs to the Patients

“The idea that patient data belongs to providers or vendors is an epic misunderstanding. Patient data belongs to patients” – Seema Verma, Administrator CMS
CMS released proposed rules that require many types of insurers to provide electronic health data in a standard format by 2020. These rules require healthcare providers and health plans to implement open data-sharing systems to ensure data can easily flow from one system to another, potentially by way of patient apps.
The major goal of CMS and the Office of the National Coordinator for Health Information Technology is to empower patients to control their own healthcare data and finally put them in the driver’s seat. The healthcare industry now needs to rely on modern technology, such as the near-ubiquitous use of smartphones and mobile apps to allow patients to take command of their care by virtue of gaining further access to their data.
How Interoperability Exists Today
Various interoperability standards such as Health Level Seven (HL7) and FHIR are competent in the industry for better streamlining of health documentation and care coordination. With the help of FHIR, doctors can get access to the health data on their mobile phones through multiple API functions that FHIR supports. Ability to access accurate data from sources other than EHRs is the need of the hour.
The Curious Case of Health Data Exchange
Since 1987, HL7 International has been working on healthcare data standards to create and improve the standards in use throughout the healthcare industry.
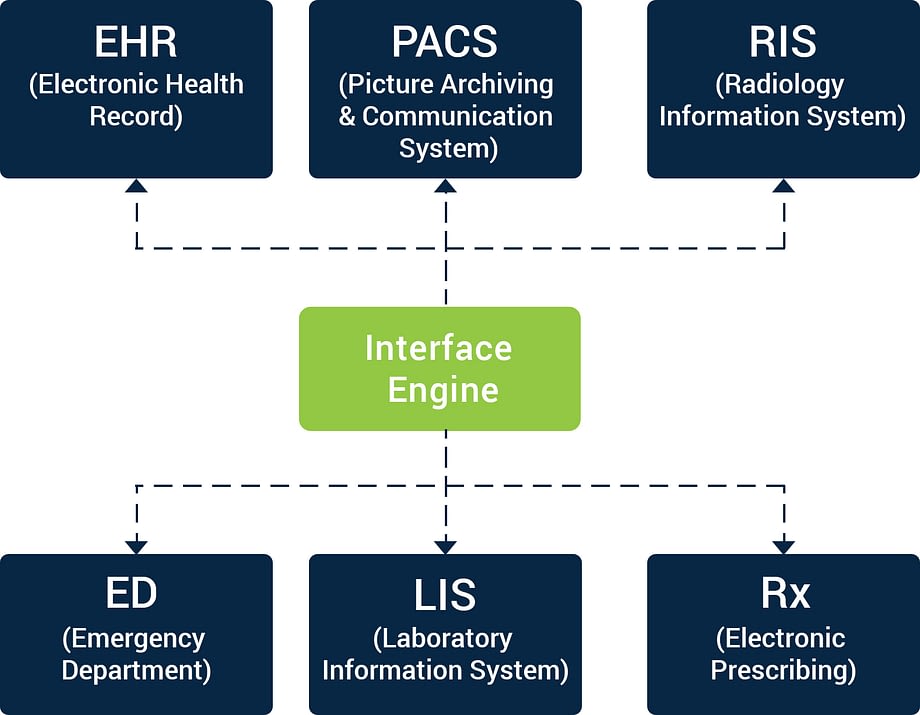
Different systems have varied workflows which are supposed to work well in a patient facility or an ambulatory environment. The technology leveraged should be flexible and easily configurable. The traditional data exchange pattern should be replaced with data exchange through an advanced integration engine.
Integration engines can act as a hub to offer seamless integration and cut down the development cost and time drastically. Integration engines are quick and simplify the workflow for central monitoring, flow control, alerting, data mapping, and more, to organize the data flow within these applications.
The Story Behind Healthcare APIs
The healthcare industry cannot optimize interoperability without creating data and adhering to data standards. The healthcare industry needs to adopt a standardized implementation model with the help of web APIs.

APIs are also being deployed within business intelligence platforms to create a centralized, 360-degree view of the patient. They represent a framework for solving complex clinical problems. The true IoT experience can be made possible with APIs where people can push the data from their medical devices directly to the medical records with ease. Multiple data sources such as genomics and lab data will be transferable. As APIs are helping these providers to offer more precise care based on all the data being accumulated from APIs coming in from apps and hardware.
SMART on FHIR
Developed by Boston Children’s Hospital and Harvard Medical School Department of Biomedical Informatics in 2010, and SMART on FHIR is immensely supported by the healthcare industry. It focuses on three key areas.
📌 Guide the client to have a review of them and negotiate access to data in the EHR
📌 Provide guidelines as to how the data will be exchanged and how a person can access it (With the help of FHIR REST API)
📌 Provide a medium to launch external apps through the EMR

SMART on FHIR addresses the needs of end-users and app developers while providing an open-standards-based platform that aligns with the needs of clinical system vendors. To build upon the momentum, we recommend a strong push towards early platform adoption in service of business cases that provide value today.

Will the Hybrid Approach to Data Exchange Work?
On-premise EHRs and cloud use should be combined with the modern FHIR API approach to data exchange. But to bring this hybrid approach to data exchange into reality, we require an extremely flexible, platform approach to manage the health data. To help guide the flow of data between applications and systems (regardless of database location), we need centralized command systems at the core. It will ensure that each application and healthcare provider have the right patient data, with the right insights, at the right time.

Here are some more examples leveraging Semantic Interoperability to advance health data exchange.
Data Hosting, Management, and Support/Cloud Service

Hospital Information & Communication Systems

Consumer Device Management & Supply

The Road Ahead
Today’s patients are smart and actively engaging their own health data and influencing care decisions. When it comes to the health data, the new rules proposed by CMS have given the steering wheel in the hands of patients. Seamless and secure data exchange is the need of the hour to ensure the right care, at the right time, to the right person and at the right cost.
Healthcare technology developers should seek input and collaboration with federal agencies to inform governance implementation and ensure broad participation. Modern-day health data exchange strategies need to be leveraged while welcoming advanced health data exchange standards like FHIRs to take a step further towards a universally interoperable healthcare ecosystem.
This eBook can help you look holistically at advanced and secure data sharing strategies that span the entire patient care continuum.

Comments
Post a Comment