Within the healthcare sector, quality is a critical factor towards keeping a healthcare organization afloat. Effective care delivery is heavily reliant on the quality and speed of execution. To address these two parameters, there have been significant and consistent innovations in the healthcare sector. While the industry progresses further along its digital evolution course, there is a heightened level of communication between patients, healthcare specialists, devices and data generation. This technological advancement of digitization brings with it the need for Quality Assurance (QA) and testing, which is integral to identifying the benefits of innovation, performing advanced analytics, making sound investments, and improving the overall performance of the healthcare software product. Accuracy and precision are impossible to achieve without a stringent system of QA and testing.
Core Aspects
- Quality Assurance: This is the process of ensuring and maintaining quality consistency through a consistent process of performance measurement, which enables optimum performance levels of healthcare software products.
- Quality Control: A quality control process is the establishment of specific protocols that aid the healthcare organization to elevate the quality of service and care provided. Quality control programs prioritize the patient and ensure overall effectiveness.
- Testing: A method through which every enhancement and installation are rigorously tested to gauge performance quality and ensure smooth functioning. This process ensures that benchmarks are consistently met.
What are the Testing Challenges in Healthcare Application?
Challenge #1: Addressing the Versatile Needs of Multiple Users
- Software usability needs to be holistic in its approach to address the requirements of one and all.
- A healthcare software application, for example, must address the specific needs of patients, caregivers, insurers, administrative staff and every other stakeholder involved. The testing process, therefore, has to be approached from multiple angles to ensure overall usability. At the outset, QA specialists need to comprehend and analyze basic and specific user requirements. For example, a patient’s requirement may be to track health progress on their mobile application, an insurer may look to track patient records and claims, a physician may require consistent reviews of treatment progress, and administrative staff may need to automate office processes.
- Each requirement can be tested separately or holistically for overall satisfaction.
Challenge #2: Setting the Standard for Security
- Compliance with Health Insurance Portability and Accountability Act (HIPAA) is not only mandatory, but a sure shot method to keep software safe and maintain security protocols.
- Primarily, HIPAA is a regulatory requirement that concentrates on the security and privacy of all health-related data, but also requires specific domain knowledge from QA specialists. Every QA procedure needs to be thoroughly HIPAA compliant with this act and comprehensive knowledge of it is an important requirement during QA and testing.
- Areas, such as authenticity and authorization, accessibility and data usage, encryption and transfer protocol, auditing and structuring are all essential components of testing towards HIPAA compliance. If the standard is set towards HIPAA compliance, the quality specialists can rest easy knowing that security standards are satisfactorily met.
Challenge #3: Interoperability Standards and Process Adherence
- Data transfers are required to comply with certain standards, such as Fast Healthcare Interoperability Resources (FHIR), Health Level Seven (HL7), and Digital Imaging And Communications In Medicine (DICOM). These standards range across data transfers between mobile applications, standard stations, EHR systems, etc.
- FHIR is a standard framework to simplify interface building with Application Programming Interface (API). For effective operation, this standard has to be widely adopted across multiple applications within the organization. HL7 is a standard requirement for the exchange, retrieval and merging of health data that ensures data transfer is accurate, through comprehensive testing of communication modules with tools like MQF Validation Tool, NIST Message Validator, Message Workbench, etc. Finally, DICOM is an international standard for efficient and safe medical image viewing, storage, processing, sharing, and analysis.
Types of Healthcare QA

1. Functional Testing
This form of testing addresses the functional capabilities of healthcare applications, including testing of healthcare workflows across the enterprise through Integrated Health Enterprise (IHE) that works to improve information sharing processes.
2. Conformance Testing
Testing conformance to healthcare industry frameworks and security requirements (e.g. Meaningful Use, HIPAA, FDA requirements, VA requirements) come under conformance testing that ensures security protocols are met.
3. Interoperability Testing
Another form of conformance testing is the measurement of interoperability standards (e.g. HL7, FHIR, DICOM, NCPDP, CCD/CDA) by using industry-standard testing tools. This is a measure of the security levels adopted during data exchange, according to regulatory requirements.
4. Medical Imaging Testing
The security and accuracy of the medical imaging software are undertaken through testing medical imaging applications, including specialized test automation tools for medical imaging, such as MESA, DVTK, and Mirth.
5. Platform Testing
This includes the rigorous testing of software on mobile platforms and mobile applications for iOS, Android, Windows, etc. Another dimension of testing is the measurement and effectiveness of cross-browser compatibility.
6. Load and Performance Testing
Testing enterprise healthcare applications against load and performance benchmarks through leveraging cloud platforms, such as Azure, Amazon EC2, and Google to ascertain the capability of managing load and performance output.
Best Practices for Healthcare QA
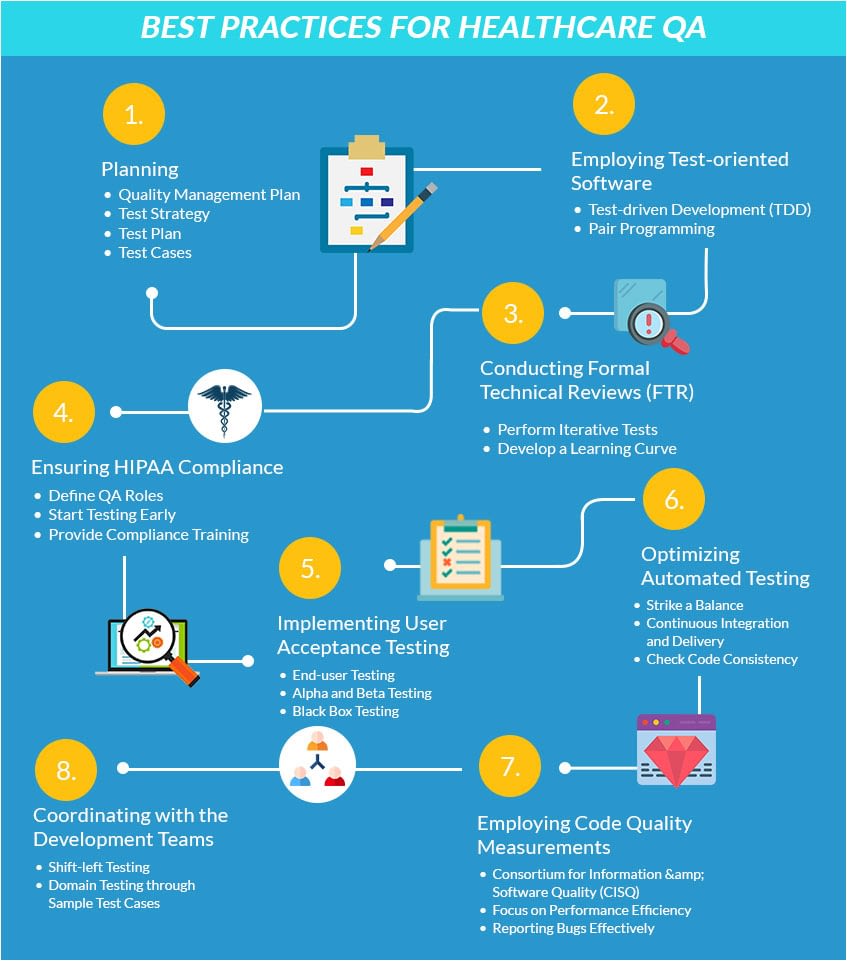
1. Planning:
- Quality Management Plan – This includes the gauging of the means through which quality levels will be consistently adhered to throughout the execution of the custom healthcare software development process and the testing procedures for the same.
- Test Strategy – A clear understanding and outline of the testing procedures and strategies should be charted out from the outset, along with a detailed communication across the QA and testing team.
- Test Plan – This is the actual testing plan that needs to be put into operation. It should detail the multiple tests that are required towards the specific software and the frequency of testing that needs to be undertaken.
- Test Cases – Case studies should be recorded for reference and every testing procedure should be documented for easy referral. Test cases help with present testing procedures and provide an insight for future development testing.
2. Employing Test-oriented Software
- Test-driven Development (TDD) – This practice is one where developers write the code based on the automated tests to avoid duplication of codes and allow for continual testing during development, as opposed to testing after the code is written. For further information on the details of TDD, please refer to How to Implement DevOps in Healthcare.
- Pair Programming – This process is an intensive programming approach, wherein two programmers work together on a single machine. One programmer undertakes writing the code and the other one is simultaneously undertaking QA and testing and making suggestions for improvement.
3. Conducting Formal Technical Reviews (FTR)
- Perform Iterative Tests – This form of testing is undertaken iteratively, wherein a risk-based approach is adopted to identify significant testing assets and reducing bugs and delays from the outset.
- Develop a Learning Curve – Through this QA activity, functional errors are speedily recognized, standard adherence is ensured, security requirements are continually highlighted, pre-defined standards are clearly outlined, and uniformity is established among multiple developers.
4. Ensuring HIPAA Compliance
- Define QA Roles – This is a clear outline and representation of the roles of various testers in the larger scheme of things that establishes testing clarity and reduces overlap or lapses among multiple testers.
- Start Testing Early – Testing should not be undertaken as a simultaneous process through the development and not after the development process is complete. A dedicated QA team should be placed at the outset and should operate in tandem with the developers.
- Provide Compliance Training – A thorough orientation of the standards and protocols of all regulatory and compliance requirements should be undertaken, along with continual reorientation planning for strict adherence.
5. Implementing User Acceptance Testing
- End-user Testing – This is the process of adopting a strategy where testing is undertaken to determine the usability of the software from the perspective of the end-users requirements.
- Alpha and Beta Testing – These forms of testing are adopted at the development and pre-release stages and involve the testing of regulatory requirements and production readiness.
- Black Box Testing – This is the process of examining the functionality of the healthcare software product, without the measurement of the internal code. It analyses the development from the perspective of the user and not the developers.
6. Optimizing Automated Testing
- Strike a Balance – There are individual benefits to manual testing and automated testing and a combination of both can provide optimal results. Executing automated testing procedures, wherever appropriate, can reduce manual testing time.
- Continuous Integration and Delivery – This method ensures that testing and QA is conducted simultaneously along the development process and is not an after-thought, which requires significant rework.
- Check Code Consistency – The consistency of the code should be examined across the entire spectrum of the healthcare solution module level and complete solution-level to ensure maximum effectiveness.
7. Employing Code Quality Measurements
- Consortium for Information & Software Quality (CISQ) – This approach ensures the comparison and contrast of the custom healthcare software quality model to provide an overall purview of benefits, weaknesses, and costs involved.
- Focus on Performance Efficiency – When QA and testing procedures are executed the priority should remain on the performance efficiency of the development from the user’s perspective.
- Reporting Bugs Effectively – QA and testing methods should factor in the effective reporting of bugs, along with detailed information for quick remedial action by the developers.
8. Coordinating with the Development Teams
- Shift-left Testing- Executing the testing phase as early as possible in the healthcare software development process is an agile practice that involves the prioritization of the testing process as an early or simultaneous part of the development process. For more information, please refer to How to Implement DevOps in Healthcare.
- Domain Testing through Sample Test Cases – Creating test case samples of multiple arenas of testing, such as provider systems, member systems, claims management systems, regulatory compliance, and performance testing will help the specialists promptly identify problem areas.

Can BA/QA integration transform Modern Healthcare Development?
- The close working of Business Analyst (BA) and Quality Analyst (QA) allows for testing to be conducted during the building.
- It further allows for an enhanced level of alignment between multiple related individuals that contribute to cross-functionality and integration.
- Product and process expertise go hand in hand to provide optimal results, as opposed to remote goals that lie bereft of holistic value.
- This method further allows developers to work at a faster rate through quicker approvals and identification of required modifications.
- Business requirements and goals are clearly communicated and promptly executed from the BA to the developer, and thereafter by the QA.
Conclusion:
Adopting agile techniques, compounded with the simultaneous association of developers, business experts, and QA specialists will improve efficiencies across the organization and provide higher quality healthcare software products. This model of integration and the adoption of smart testing methods reduce gaps and increases end-user satisfaction through cross-functionality.
This model of integration and the adoption of smart testing methods reduce gaps and increases end-user satisfaction through cross-functionality.
Comments
Post a Comment