The importance of Artificial Intelligence is often understated and also overstating the same is quite difficult.. to get in-depth with how AI is actually bringing changes in MCA, we must get to the basics of what Medical Billing and Coding really are.
MEDICAL CODING
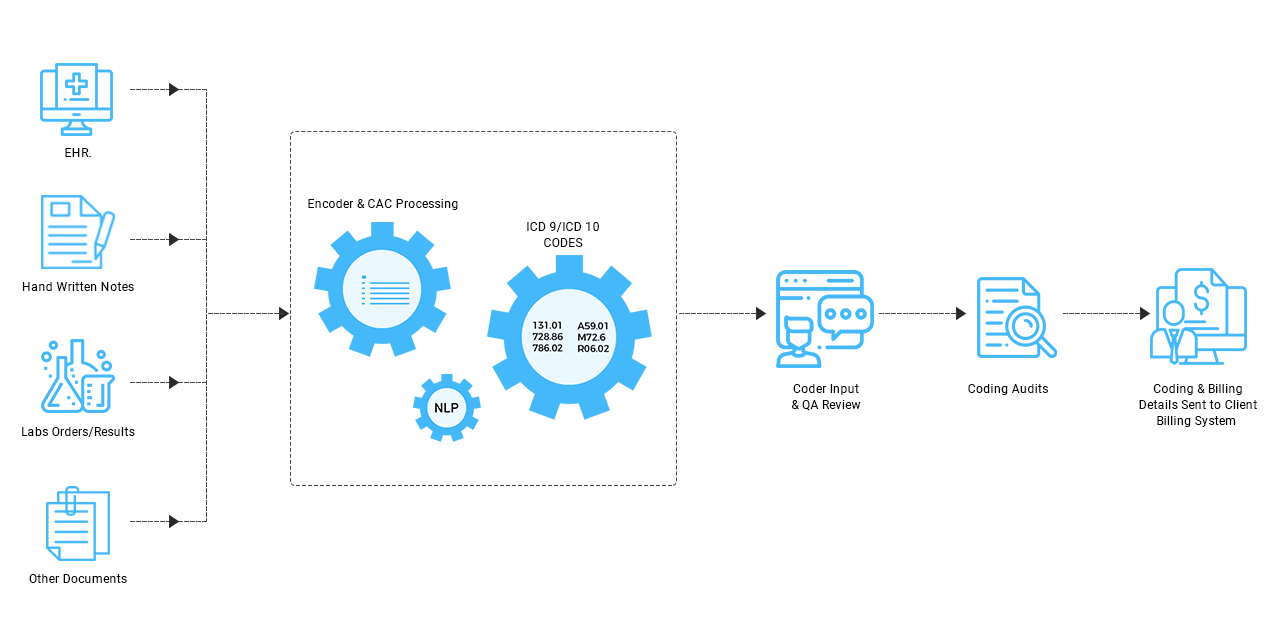
Medical coding system, if we talk about it at a very basic level -- is something that a coder takes, a written piece if you may, and translates it as accurately as possible into a coded format such as numeric or alphanumeric code. The piece that's taken for translation can be something such as a prescription for medication or a doctor's diagnosis or something else medical related. A code for each and every event is created, these events can be of injuries, diagnosis or Compliant Coding Software Solutions
Presently, there are about a hundred thousand codes existing that are used for medical procedures, outpatient procedures, and diagnoses. Let us have a look at a simple example of Medical Coding:
Let's say that a patient has walked into a doctor’s office and he/she is coughing tirelessly, they have a high production of mucus, and have a dreaded fever. Then a nurse walks up to the patient and asks them their symptoms, once the symptoms are noted, she performs some initial tests to get an idea of what is actually going on, and then comes the doctor who analyzes and concludes the diagnoses saying that the patient is suffering from bronchitis. A medication is then prescribed to the patient by the doctor.
Now comes the interesting part of Modern Healthcare, each and every part of the visit is recorded by the clinic be it the doctor or someone in the office who is authorized to carry out such operations. Then begins the coders job that is to translate all of the relevant information of the visit into numeric and alphanumeric codes, which are ultimately used in the billing process.
The clinical coding solutions should be equipped with the knowledge of a few sets and subsets of code, let's take two of the subsets: International Classification of Diseases (ICD) these codes correspond to a patient’s injury or sickness, and Current Procedure Terminology (CPT) that are related to the functions and services Healthcare providers perform to the patient this can be as performing on them and performing for them.
A task included for the Medical Coders is to translate every bit of data or information of the patient's visit to the clinic and shape it in the form of a code. There are different codes for different kinds of visits, some codes are more specific these specific codes can be such as the patients symptoms, the tests performed by the doctor and the diagnosis procedure used by the doctor.
The Medical Coders have to keep these guidelines in mind, they are very important and can affect the status of a claim. The coding process concludes when the Medical Coder has entered the proper codes into the for or software program. This is where the job of the Medical Coder ends, now, all of this is passed on to the Medical Biller.
Comments
Post a Comment