As well as you recognize, hospitals, clinics, and bigger healthcare systems are known to save lives and treat patients with care. However, to make sure that it's done properly, every healthcare organization must create successful processes and policies to remain financially healthy and to stay constant in their work by doing their best.
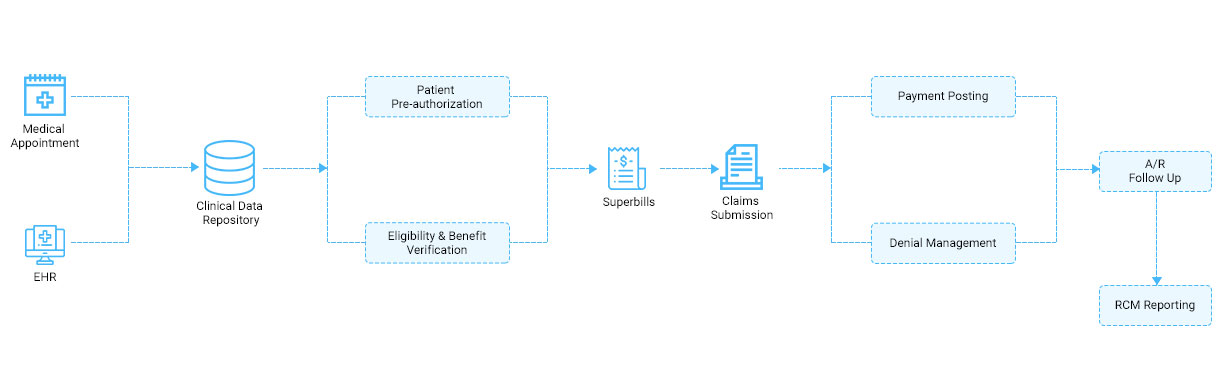
Hence, comes revenue cycle management software into the picture. In the field of healthcare, RCM works as the financial process facilitating the management of clinical and administrative functions associated with claims processing, payment, and revenue generation. The process covers identifying, managing, and collecting patient service revenue. All in all, Healthcare revenue cycle management is the strategy used by the healthcare organization to save their medical organization time and money. RCM makes it possible to get more money per patient, quickly, with lesser wasted efforts.
Today’s revenue cycle system processes are quite complex. With the help of a knowledgeable medical billing company, there's guaranteed economic success and compliance with many government regulations. Billing is no longer something that any staff can do once they have time between patients. The disputes of the interior billing operations can cause collection shortfalls and non-compliance issues. That's why outsourcing to a knowledgeable Practice Management/Billing company makes it sensible.
The main features of Revenue Cycle Management are:-
1. Available Via the Cloud
This is one of the best features for you to consider while implementing revenue cycle management software is cloud computing. This reduces the pressure of your IT department since they will no longer have to predict how much server space or bandwidth is needed to access the RCM data.
2. Complete Training
Verify with the software provider that they provide comprehensive RCM training on using the system for any functions you want to perform. Usually, you'll coach your most knowledgeable and computer-savvy employees first since they're going to take less time to urge and hurry up and that they can then help fill in gaps of data with fellow workers after they’ve been trained.
3. Submit Claims at its best Value
Prudent office managers know that it's more efficient to figure out with an RCM that gives the power to make sure claims are submitted at their highest possible value before being submitted. This is often very true once you are watching potential reductions in reimbursements.
4. Checking Eligibility
Your healthcare revenue cycle management solutions help with these eligibility inquiries, taking care of knowledge transactions online. This saves time from when the staff would rather be hanging on the phone, expecting a response from the patient’s provider.
5. Claim Tracking and Correction
When a busy employee happens to cause a typo or chooses the incorrect code for a bill, you don’t want to attend an undue amount of your time just to take care of the error . One among the simplest RCM features at your disposal are going to be the power to trace submitted claims in real-time and to see their status. When a drag is detected, your employees are going to be given the chance in the RCM to quickly edit and resubmit any of those denials.
6. Alerts for Denials
Of course, the simplest way to avoid denials in the first place is to line up your RCM with pro-active denial alerts. Each member of your team will now have the power to re-code anything that’s been alerted. If an RCM cannot tell when data is wrong , it slows down worker productivity and may start the flow of revenue in your organization.
7. Key Performance Indicators and Reports
Preparation for the weekly meetings where staff gets together to travel over reports will go far more smoothly and quickly once you find out your RCM to get reports, including documentation for shielding Access to Medicare Act, or PAMA, alongside financial and managerial reports.
Comments
Post a Comment