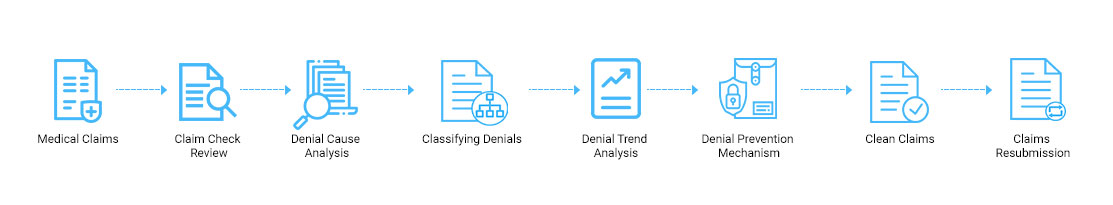
Maintaining Denial Management has become a daunting task in today's era. If claims are denied, it could cause a significant impact on hospitals and healthcare professionals. For every patient, there are some other challenges he/she needs to face. Claims denial management deals with unpaid claims and is considered an essential aspect of revenue cycle management. It can swiftly pinpoint why the shares are being denied to prevent mistakes again. Healthcare Providers face unique challenges from the patients. Every claim is individual for each patient. Denial Management includes the creation of specific procedures for appealing the denial of medical claims. It is one of the crucial elements which ensures steady cash flow. Services include the fundamental problems causing claims denials, classifying its source and cause, and developing effective strategies to prevent it. Some challenges of Denial Management need to be overcome.
Rising Challenges of Denial Management
1. The rising issue of Patient Responsibility
Some high deductible health plans for the patients who share responsibilities for payments cause more pressure. As prices continue to increase, it becomes tough to gather the payments on time. Some resolution programs are going in a place that seeks revenue cycle vitality.
2. Need Proper Strategies for Denial Management
Some of the practices which are carried out are still paper-based processes that are less efficient and organized. These processes do not have the same automation support that virtual systems possess. The result is non-optimal for Denial Management in Healthcare.
3. Value-Based Care denials influence the profitability of Revenue Cycle Management.
While value-based care denials have positive implications, it leads to severe impacts on standardized payments and denial management costs.
4. Complexity is causing more rise in Denial Claims
There are some complex requirements in insurance companies that cause practices to deal with initial denials. The rework which is done to the denial claims and appeals hinders the revenue cycle improvement initiatives.
How to overcome these challenges?
1. With the help of data analytics, one could find out the root problems in denial claims. One must also find the initial denial rate and figure out the best solution. Once it has been identified, one must discover who has impacted most, whether it is the payer or the healthcare providers. The clinical and the revenue cycle management areas should be completely redesigned.
2. One must investigate registration and the pre-service issues. Denial Management in Medical Billing claims occur when the payer isn't responsible for the coverage. It's the front desk duty to pay attention and confirm the patient's eligibility beforehand. The preauthorization process will get managed by the payers and plan for the claim. It also includes a medical denial account related to a certain percentage of the denials at the heart of failure if authorization is not done on time.
3. All the information should be gone from the provider to the payers and then back to the healthcare providers. Providers improve efficiency by having clinical guidance and evidence which solves complex cases.
4. Automating the entire process makes it easy for the staff to verify everything and provide a smooth, streamlined process. Automation should also be done in the payer's maintenance policy in every location, which helps raise accuracy to lower the admin work. The staff has to ensure all the operational reports like revenue and finance cycle should get circulated and reviewed regularly, providing a clear path on which one to focus. It will help the health practice to ensure the future denials won't happen.
Comments
Post a Comment